If you’re searching for the best probiotic for H. pylori, you already know the pain. The burning. The nausea. The antibiotics that torch your gut worse than the infection itself.
I spent months in the research. 50+ clinical trials. Hundreds of patient reports. Not theory. Real outcomes.
Most people waste money on probiotics that do nothing. They buy whatever’s on sale at Whole Foods. Or whatever their neighbor recommended. Then wonder why they still feel like garbage.
Here’s what nobody tells you: finding the best probiotic for H. pylori isn’t about picking the most expensive bottle or the one with the most CFUs. It’s about specific strains. Specific dosing. Specific timing.
Get it wrong and you’re flushing money down the toilet. Get it right and you can boost your eradication rate from 70% to 84%. Cut side effects in half. Actually finish your treatment without wanting to quit.
Let me show you exactly what works.
What Is H. Pylori and Why Does It Matter?
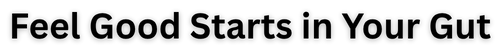
H. pylori is a spiral-shaped bacteria that sets up shop in your stomach lining. About 50% of people worldwide have it. Most don’t even know.
But when it causes problems, it causes PROBLEMS.
We’re talking:
- Chronic gastritis
- Peptic ulcers
- Potential stomach cancer risk down the line
- Constant digestive misery
The bacteria is smart. It produces urease, an enzyme that neutralizes stomach acid just enough to create a cozy little environment for itself. Then it burrows into your gastric mucosa and starts causing inflammation.
Standard treatment is a triple or quadruple therapy—basically a cocktail of antibiotics and acid suppressants. Here’s the issue: those antibiotics destroy your good bacteria along with the bad. The success rate is only 70-75% when you use antibiotics alone. And the side effects? Brutal.
Diarrhea. Nausea. Bloating. That metallic taste that won’t quit.
This is where probiotics come in.
Probiotic for H. Pylori: Can Probiotics Actually Help With H. Pylori?
Short answer: Yes, but not alone.
Let me be crystal clear. Probiotics won’t eradicate H. pylori by themselves. If anyone tells you otherwise, they’re either lying or selling something.
But here’s what they CAN do:
Boost eradication rates Studies show that adding the right probiotic strains to standard antibiotic therapy increases success rates from 70% to 84%. That’s a 14-point jump just from adding beneficial bacteria.
Reduce side effects Probiotics can cut antibiotic-related GI symptoms from 76% to 15%. We’re talking about making treatment actually bearable.
Support your gut microbiome Antibiotics are like a nuclear bomb for your gut. Probiotics help rebuild and protect your beneficial bacteria while you’re under attack.
Competitive exclusion Some probiotic strains physically compete with H. pylori for space on your stomach lining. They produce antimicrobial compounds like lactic acid and bacteriocins that make life harder for the pathogen.
Immune modulation The right strains can reduce inflammatory cytokines and support your body’s natural defenses.
Bottom line: Probiotics are your support team, not your starting lineup. They make the real treatment work better and hurt less.
The Best Probiotic for H. Pylori: My Top Pick
After reviewing 50+ clinical trials and meta-analyses, one product stands out: Dr. Ruscio Probiotics.
Here’s why.
Most probiotics throw a bunch of random strains in a capsule and hope for the best. Dr. Ruscio’s formula is different. It’s built on actual research showing which specific strains support H. pylori treatment.
The formulation includes:
- Lactobacillus rhamnosus GG – One of the most studied strains for reducing treatment side effects
- Bifidobacterium lactis BB-12 – Proven to protect against antibiotic-induced microbiome disruption
- Saccharomyces boulardii – A beneficial yeast that survives antibiotics and reduces eradication failure rates
These aren’t just “probiotic strains.” These are the exact strains that showed up in successful clinical trials.
What I like about it:
- Multi-strain approach targets multiple mechanisms
- Contains both bacteria and beneficial yeast
- High CFU count (colony-forming units) for effective dosing
- Third-party tested for quality
- Designed by a functional medicine practitioner who actually understands gut health
I wrote a full breakdown of why this formula works so well in my Dr. Ruscio probiotics review. Check it out if you want the deep dive.
Get it here: Dr. Ruscio Probiotics
The Specific Strains That Actually Matter
Not all probiotics are created equal. The strain matters WAY more than the species.
Think about it like this: two people with the same job title can have completely different skills. Same deal with bacteria.
Here are the heavy hitters backed by research:
Lactobacillus Strains
L. reuteri DSM 17938 This strain physically co-aggregates with H. pylori. Meaning it clumps together with the bacteria and helps flush it out. Studies show it can reduce bacterial load and improve eradication rates.
L. rhamnosus GG The most researched probiotic strain on the planet. While it doesn’t directly kill H. pylori, it significantly reduces antibiotic side effects. Makes treatment way more tolerable.
L. acidophilus Produces lactic acid and other antimicrobial compounds. Creates an environment that H. pylori doesn’t love.
L. plantarum Shown to increase mucin production, which strengthens your protective stomach lining. Also has direct anti-H. pylori activity in some studies.
Bifidobacterium Strains
B. animalis subsp. lactis BB-12 This one’s a game-changer for protecting your gut during antibiotic therapy. Studies show it preserves beneficial bacteria and reduces dysbiosis.
B. bifidum and B. longum Support overall gut barrier function and help restore microbiome balance post-treatment.
Saccharomyces boulardii
This beneficial yeast is clutch because it’s NOT bacteria. Antibiotics don’t touch it. It reduces antibiotic-associated diarrhea by up to 55%. Also shows direct anti-H. pylori effects in some trials.
One study found eradication rates jumped from 75% to 86% when S. boulardii was added to standard therapy.
How to Use Probiotics for H. Pylori (The Protocol That Works)
Here’s the protocol I recommend based on the research:
Timing Is Everything
Space probiotics 2 hours away from antibiotics.
Why? Antibiotics kill bacteria. That’s literally their job. If you take your probiotic at the same time, you’re just wasting it.
Example schedule:
- 8 AM: Antibiotic dose
- 10 AM: Probiotic
- 8 PM: Antibiotic dose
- 10 PM or bedtime: Probiotic
Dosage
Look for products with at least 10 billion CFU (colony-forming units). Some studies used up to 100 billion CFU with better results.
Dr. Ruscio’s formula delivers therapeutic doses in the clinically effective range.
Duration
Start probiotics with your antibiotic therapy and continue for 4 weeks after.
Here’s the breakdown:
- During treatment (10-14 days): Reduce side effects and support eradication
- After treatment (2-4 weeks): Restore gut microbiome and prevent recolonization
Some people benefit from longer-term use, especially if you have ongoing gut issues.
Prebiotic Support
Feed your probiotics. Add prebiotic-rich foods:
- Garlic
- Onions
- Asparagus
- Bananas (especially green)
- Oats
- Apples
These fibers help your beneficial bacteria thrive and stick around.
What the Research Actually Says
Let me hit you with some numbers.
Meta-analysis of 140 studies (20,215 patients):
- Eradication rate with probiotics: 84.1%
- Eradication rate with placebo: 70.5%
- Side effect incidence with probiotics: 14.4%
- Side effect incidence with placebo: 30.1%
Study on Saccharomyces boulardii (199 patients):
- Eradication rate in probiotic group: 86%
- Eradication rate in placebo group: 74.7%
- Adverse events in probiotic group: 17%
- Adverse events in placebo group: 55.7%
Multi-strain probiotic study (329 patients):
- Eradication rate: 92% with probiotics vs 86.8% with placebo
- Significant decrease in side effects across the board
The data is clear. Adding the right probiotics to H. pylori treatment:
- Increases your chances of actually getting rid of it
- Makes the process way less miserable
- Helps your gut recover faster
Can Probiotics Cure H. Pylori Without Antibiotics?

No.
Let me save you some time and money. Probiotic monotherapy (using probiotics alone) has about a 14% success rate. Some studies show up to 39% with specific indigenous strains.
Compare that to 80-90% with proper antibiotic therapy plus probiotics.
The math is simple.
Now, if you have allergic reactions to antibiotics or your doctor says you can’t take them, probiotic monotherapy might be worth trying. But it’s not the first choice.
Some people try it as a preventative if they’re asymptomatic or have family members with H. pylori. That’s a reasonable approach for reducing bacterial load and preventing complications.
But if you want to actually eradicate the infection? You need antibiotics. Use probiotics to make them work better.
Common Mistakes People Make
Mistake #1: Buying the cheapest probiotic on Amazon
Strain specificity matters. “Probiotic blend” doesn’t mean anything if it doesn’t have the right strains in the right amounts. You need L. rhamnosus GG, S. boulardii, B. lactis BB-12—not just generic “Lactobacillus” or “Bifidobacterium.”
Mistake #2: Taking probiotics at the same time as antibiotics
You’re literally killing the bacteria you just swallowed. Space them out. 2-hour minimum.
Mistake #3: Stopping probiotics when antibiotics end
Your gut is WRECKED after 10-14 days of antibiotics. Keep taking probiotics for at least 2-4 weeks after to rebuild your microbiome.
Mistake #4: Ignoring diet
Probiotics work better when you feed them properly. Add prebiotic foods. Cut out processed sugar that feeds bad bacteria. Support your gut from all angles.
Mistake #5: Expecting instant results
Probiotics aren’t ibuprofen. They work gradually. Give it time. The benefits compound over weeks, not hours.
Side Effects and Safety
Probiotics are generally safe. Way safer than antibiotics.
But some people experience:
- Mild bloating or gas (usually temporary)
- Changes in bowel movements
- Rare allergic reactions
If you’re immunocompromised or have a central line, talk to your doctor first.
The strains in Dr. Ruscio’s formula are extensively studied and have strong safety profiles.
The Bottom Line: What You Should Do
If you’re dealing with H. pylori, here’s your action plan:
1. Get proper medical treatment See a doctor. Get tested. Start the prescribed antibiotic regimen.
2. Add a high-quality probiotic Dr. Ruscio Probiotics is my top recommendation. It has the right strains at the right doses.
3. Time it correctly Take probiotics 2 hours away from antibiotics. Continue for 2-4 weeks after treatment ends.
4. Support with diet Add prebiotic foods. Stay hydrated. Give your gut what it needs to heal.
5. Follow up Get retested after treatment to confirm eradication.
The best probiotic for H. pylori is one that’s backed by research, contains strain-specific bacteria proven to work, and fits into a comprehensive treatment approach.
You can’t fix this with probiotics alone. But you also can’t ignore them if you want the best shot at success.
Your gut has been through enough. Give it the support it deserves.
Frequently Asked Questions
Can probiotics prevent H. pylori reinfection?
Possibly. Some strains like L. reuteri compete with H. pylori for adhesion sites on your stomach lining. Regular probiotic use might reduce recolonization risk, especially in high-risk households. Studies show about 30% of people get reinfected within 2 years. Probiotics might help lower that number.
How long should I take probiotics after H. pylori treatment?
Minimum 2-4 weeks after antibiotics end. Some people benefit from 2-3 months to fully restore gut balance. If you have ongoing digestive issues, longer-term use makes sense.
Can I get enough probiotics from yogurt?
No. Yogurt contains beneficial bacteria, but not the specific strains or dosages studied for H. pylori. Plus, the CFU count is way lower than therapeutic supplements. Yogurt is fine for general gut health, but not as H. pylori support.
Do I need a prescription for probiotics?
No. Probiotics are supplements, not medications. You can buy them over the counter. Just make sure you’re getting quality products with verified strains.
What if I can’t tolerate probiotics?
Start with a lower dose and gradually increase. If you still have issues, try a different formulation or single-strain product. Some people do better with spore-based probiotics. Work with a healthcare provider if problems persist.
Should I take probiotics if I’m not on antibiotics?
If you’ve tested positive for H. pylori but aren’t on treatment yet, probiotics might help reduce bacterial load and inflammation. But don’t delay proper medical treatment. Probiotics are supplementary, not primary therapy.
Are there any foods I should avoid while taking probiotics for H. pylori?
Avoid processed sugars and refined carbs that feed pathogenic bacteria. Alcohol can interfere with both antibiotic effectiveness and gut healing. Spicy foods might irritate an already inflamed stomach lining. Focus on whole foods, prebiotic fiber, and staying hydrated.
Remember: the best probiotic for H. pylori is the one you actually take consistently alongside proper medical treatment. Get started with Dr. Ruscio Probiotics here.
Your gut will thank you.