Look, I get it.
You’ve been dealing with gut issues for months (maybe years).
One day you’re fine, the next you’re doubled over in pain.
Your stomach feels like it’s staging a revolt against you.
And everyone keeps saying “it’s just stress” or “eat more fiber.”
But deep down, you know something’s off.
After treating thousands of patients with gut issues, I can tell you this: the signs of irritable bowel syndrome aren’t always what you’d expect.
Some are obvious. Others fly under the radar.
And missing them costs you years of unnecessary suffering.
What Is IBS Really? (Beyond the Medical Textbook Definition)
Irritable bowel syndrome isn’t just “stomach problems.”
It’s your gut’s way of screaming that something in your digestive system has gone haywire.
Think of your intestines like a conveyor belt.
When everything’s working smoothly, food moves through at the right speed.
Your gut muscles contract in a coordinated rhythm.
Your brain and gut communicate perfectly.
But with IBS?
That conveyor belt starts jerking around unpredictably.
Sometimes it speeds up (hello, diarrhea).
Sometimes it crawls to a halt (constipation city).
Sometimes it can’t make up its mind (welcome to the mixed-type nightmare).
Here’s what most people don’t realize: IBS affects 10-15% of adults in the US.
But only 5-7% ever get properly diagnosed.
That means millions of people are walking around suffering in silence.
The 7 Most Common Signs of Irritable Bowel Syndrome
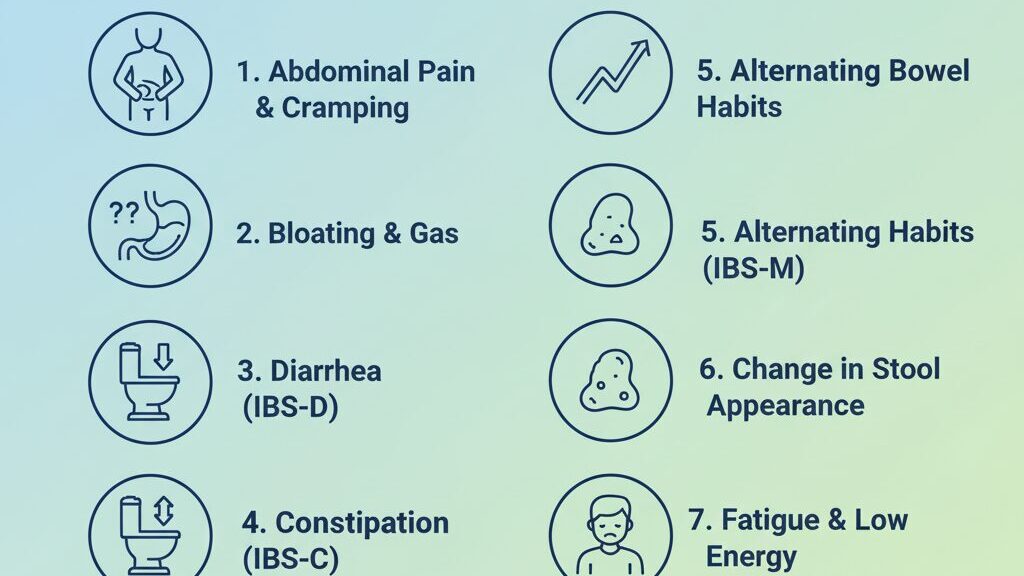
1. Abdominal Pain That Comes and Goes (Like a Bad Relationship)
This isn’t your typical stomachache.
IBS pain has a personality.
It shows up uninvited.
Hangs around for hours.
Then disappears like nothing happened.
What it feels like:
- Cramping that makes you double over
- Sharp, stabbing pains in your lower belly
- Aching that gets worse before bowel movements
- Relief after you poop (sometimes)
The telltale sign: The pain moves around.
One day it’s on your left side.
Next day it’s front and center.
Unlike appendicitis or gallbladder pain, IBS pain doesn’t have a permanent address.
2. Your Bathroom Schedule Becomes Completely Unpredictable
Remember when you could set your watch by your bowel movements?
IBS throws that reliability out the window.
You might experience:
- Going from daily poops to nothing for days
- Sudden urgent trips to the bathroom
- Feeling like you can’t fully empty your bowels
- Alternating between constipation and diarrhea
I had a patient who carried a mental map of every public restroom in her city.
That’s not normal.
That’s IBS stealing your confidence.
3. Bloating That Makes You Look 6 Months Pregnant
This isn’t the “I ate too much pizza” bloat.
IBS bloating is next-level.
You wake up with a flat stomach.
By 2 PM, you look like you’re carrying twins.
The science behind it: Your gut produces excess gas when it can’t properly break down certain foods.
This gas gets trapped, causing your belly to expand like a balloon.
The emotional toll: You start avoiding tight clothes.
You cancel dinner plans.
You feel self-conscious about your appearance.
4. Gas That Could Clear a Room (And the Embarrassment That Follows)
Let’s be honest about this one.
Everyone passes gas.
But with IBS, it becomes a full-time job.
What makes IBS gas different:
- Volume (so much more than normal)
- Timing (always at the worst moments)
- Smell (sometimes truly offensive)
- Frequency (every few minutes on bad days)
The worst part?
You never know when it’s coming.
5. Stool Changes That Would Make a Gastroenterologist Take Notes
Your poop becomes a daily mystery.
IBS-C (Constipation-predominant):
- Hard, lumpy stools like rabbit pellets
- Straining that makes your face turn red
- Feeling like there’s still more to come
IBS-D (Diarrhea-predominant):
- Loose, watery stools
- Urgency that sends you running
- Multiple trips per day
IBS-M (Mixed):
- Hard stools one day, liquid the next
- No predictable pattern
- The worst of both worlds
6. Mucus in Your Stool (The Sign Everyone Ignores)
This one freaks people out.
But it’s actually super common with IBS.
What to look for:
- Clear or white slimy coating on stools
- Stringy mucus mixed throughout
- Feeling like you’re passing pure mucus sometimes
Why it happens: Your irritated intestinal lining produces extra mucus to protect itself.
Think of it like your gut’s attempt to soothe the inflammation.
7. That “Incomplete” Feeling (Like Your Gut Has Trust Issues)
You sit on the toilet.
You push.
You think you’re done.
Five minutes later, you feel like you need to go again.
But when you try, nothing (or very little) comes out.
This is called tenesmus.
It’s your rectum sending false alarms to your brain.
Your gut basically develops trust issues with itself.
The Hidden Signs Most Doctors Miss
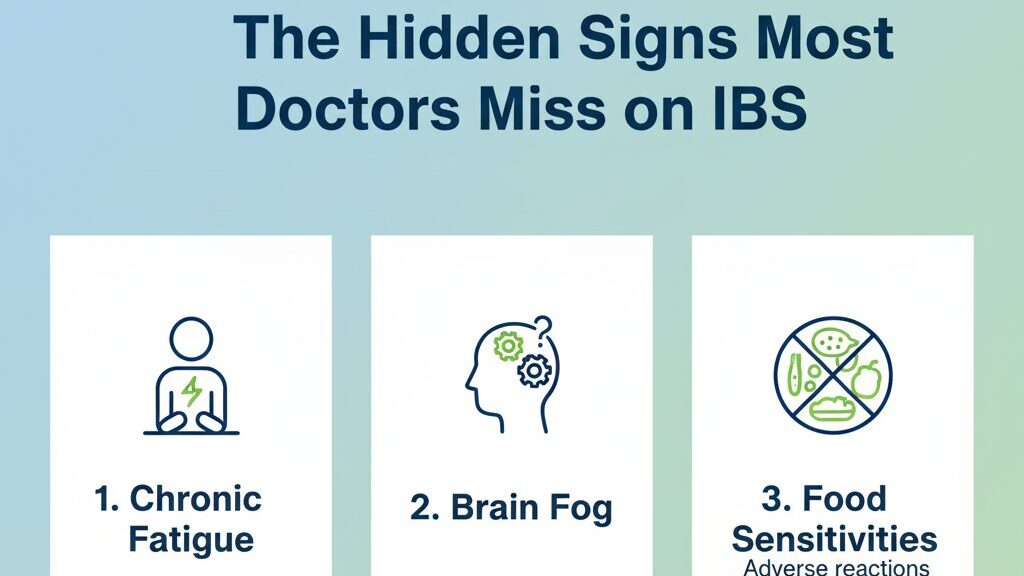
Fatigue That Feels Like You’re Running on Empty
IBS doesn’t just mess with your gut.
It drains your entire system.
Why this happens:
- Chronic inflammation exhausts your immune system
- Poor nutrient absorption leaves you malnourished
- Constant discomfort disrupts sleep quality
- The stress of unpredictable symptoms is mentally exhausting
Anxiety and Depression (The Gut-Brain Connection Is Real)
Your gut produces 90% of your body’s serotonin.
When your gut is unhappy, your brain feels it.
I’ve seen patients whose “mental health issues” completely resolved once we fixed their gut.
Common mental symptoms with IBS:
- Racing thoughts about food and symptoms
- Social anxiety around eating out
- Depression from feeling “broken” or “different”
- Panic attacks triggered by gut symptoms
Food Fear (When Every Meal Becomes Russian Roulette)
You start viewing food as the enemy.
Every bite becomes a calculated risk.
The progression looks like this:
- You notice certain foods trigger symptoms
- You start avoiding more and more foods
- Your “safe foods” list shrinks to 10-15 items
- You become malnourished and socially isolated
This isn’t healthy.
This isn’t sustainable.
This is your body crying out for proper treatment.
IBS Triggers: The Usual Suspects
Stress (The Silent Gut Destroyer)
Stress doesn’t cause IBS.
But it sure as hell makes it worse.
How stress impacts your gut:
- Slows down digestion
- Increases inflammation
- Disrupts the gut microbiome
- Triggers the fight-or-flight response
Foods That Act Like Gut Bullies
Common culprits:
- High-FODMAP foods (beans, certain fruits, wheat)
- Dairy products (if you’re lactose intolerant)
- Gluten (even without celiac disease)
- Artificial sweeteners
- Caffeine and alcohol
- Spicy or fatty foods
Here’s the thing: Your triggers might be completely different from someone else’s.
Food sensitivity is highly individual.
Hormonal Changes (Ladies, This One’s for You)
Women are twice as likely to develop IBS.
Why hormones matter:
- Estrogen affects gut motility
- Menstrual cycles can trigger flare-ups
- Pregnancy often changes IBS symptoms
- Menopause brings new digestive challenges
Medications That Mess with Your Gut
Antibiotics wipe out good bacteria along with bad.
NSAIDs (like ibuprofen) irritate the intestinal lining.
Antidepressants can slow gut motility.
Always check with your doctor, but be aware these medications can impact your digestive system.
When to See a Doctor (Red Flags You Can’t Ignore)
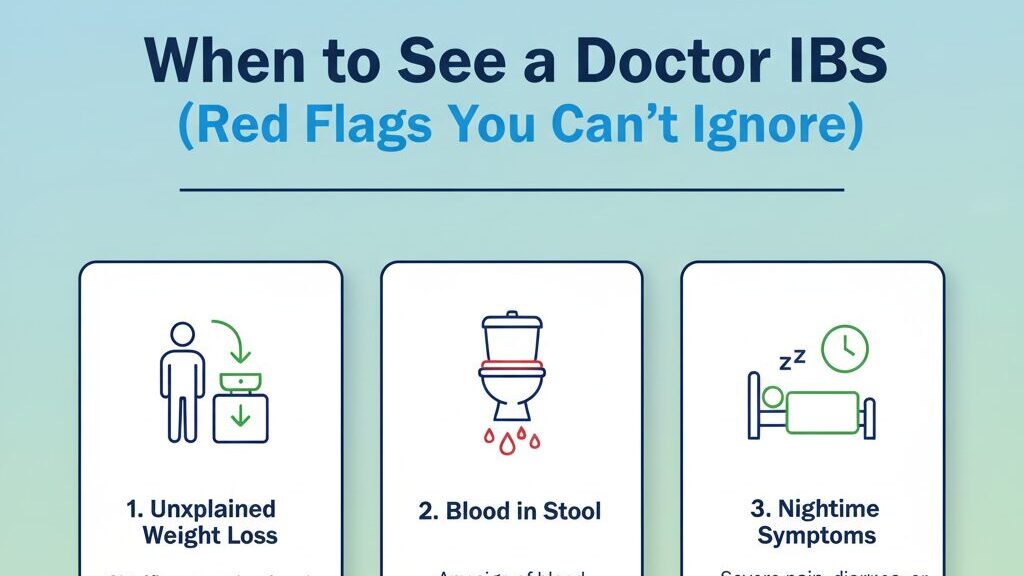
Most IBS symptoms are manageable with lifestyle changes.
But some signs demand immediate medical attention.
See a doctor IMMEDIATELY if you have:
- Blood in your stool
- Unexplained weight loss (more than 10 pounds)
- Fever with digestive symptoms
- Severe abdominal pain that doesn’t improve
- Vomiting that won’t stop
- Diarrhea that wakes you up at night
See a doctor SOON if you have:
- Symptoms that interfere with daily life
- Changes in bowel habits lasting more than a few weeks
- Iron deficiency anemia
- Family history of colon cancer or inflammatory bowel disease
The IBS Diagnosis Process (What to Expect)
There’s no single test for IBS.
It’s a diagnosis of exclusion.
Your doctor will likely:
- Take a detailed history
- When symptoms started
- What makes them better/worse
- Your stress levels and lifestyle
- Family medical history
- Physical examination
- Checking your abdomen for pain or swelling
- Looking for signs of other conditions
- Rule out other conditions
- Blood tests for inflammation or infection
- Stool samples to check for bacteria or parasites
- Breath tests for bacterial overgrowth
- Colonoscopy (if you’re over 50 or have red flags)
The Rome IV Criteria for IBS: Your doctor diagnoses IBS if you have recurrent abdominal pain at least 1 day per week for the last 3 months, with 2 or more of these:
- Pain related to pooping
- Change in stool frequency
- Change in stool appearance
My Proven 3-Step Approach to Managing IBS
After years of treating patients with gut issues, I’ve developed a system that actually works.
Step 1: Identify Your Personal Triggers
Keep a symptom diary for 2 weeks.
Track:
- Everything you eat and drink
- Stress levels (1-10 scale)
- Sleep quality
- Bowel movement details
- Symptom severity
Look for patterns.
You might discover that your Tuesday meetings consistently trigger symptoms.
Or that eating apples always leads to bloating.
Step 2: Eliminate the Obvious Culprits
Start with the big three:
- Reduce stress through meditation, exercise, or therapy
- Try an elimination diet to identify food triggers
- Improve sleep hygiene (7-9 hours per night)
Don’t try to change everything at once.
Pick one area and focus on it for 2-3 weeks.
Step 3: Rebuild and Optimize
Once you’ve removed the triggers:
- Slowly reintroduce foods to test tolerance
- Add gut-supporting supplements (probiotics, digestive enzymes)
- Build sustainable lifestyle habits
- Work with a healthcare provider for ongoing support
The Role of Diet in Managing IBS Signs
The Low-FODMAP Diet (Your Secret Weapon)
FODMAPs are certain types of carbohydrates that ferment in your gut.
For people with IBS, this fermentation creates a gas factory in their intestines.
High-FODMAP foods to limit:
- Fructose: apples, honey, high-fructose corn syrup
- Lactose: milk, ice cream, soft cheeses
- Fructans: wheat, onions, garlic
- Galactans: beans, lentils, chickpeas
- Polyols: sugar-free gum, stone fruits
Low-FODMAP alternatives:
- Fruits: bananas, berries, oranges
- Vegetables: carrots, spinach, zucchini
- Grains: rice, oats, quinoa
- Proteins: chicken, fish, eggs
Important: Don’t stay on a strict low-FODMAP diet forever.
It’s meant to be a 6-8 week elimination phase, followed by gradual reintroduction.
Fiber: Friend or Foe?
Everyone tells you to “eat more fiber” for gut health.
But with IBS, fiber can be tricky.
Soluble fiber (good for most people with IBS):
- Oats
- Bananas
- Sweet potatoes
- Chia seeds
Insoluble fiber (can worsen IBS symptoms):
- Raw vegetables
- Wheat bran
- Nuts and seeds
- Beans
My recommendation: Start with soluble fiber and add it gradually.
Your gut needs time to adjust.
The Anti-Inflammatory Approach
Chronic inflammation fuels IBS symptoms.
Foods that fight inflammation:
- Fatty fish (salmon, sardines)
- Leafy greens
- Berries
- Turmeric and ginger
- Bone broth
Foods that increase inflammation:
- Processed foods
- Refined sugar
- Trans fats
- Excessive alcohol
- Artificial additives
Lifestyle Changes That Actually Move the Needle
Stress Management (Not Just “Relax More”)
Your gut and brain are connected by the vagus nerve.
When your brain is stressed, your gut feels it immediately.
Proven stress-reduction techniques:
Deep breathing exercises (5 minutes, twice daily):
- Inhale for 4 counts
- Hold for 4 counts
- Exhale for 6 counts
- Repeat 10 times
Regular exercise (but not too intense):
- 30 minutes of walking
- Gentle yoga
- Swimming
- Cycling
Mindfulness meditation:
- Start with 5-10 minutes daily
- Use apps like Headspace or Calm
- Focus on body awareness
- Practice during symptom flare-ups
Sleep Optimization (Your Gut Heals at Night)
Poor sleep disrupts gut bacteria and increases inflammation.
Sleep hygiene basics:
- Same bedtime and wake time every day
- No screens 1 hour before bed
- Keep your room cool and dark
- Avoid large meals 3 hours before sleep
If you’re waking up with gut symptoms:
- Your dinner might be too late or too heavy
- You might have acid reflux
- Stress could be disrupting your sleep cycles
Movement and Exercise (The Gentle Approach)
Exercise helps gut motility and reduces stress.
But high-intensity workouts can worsen IBS symptoms.
Best exercises for IBS:
- Walking after meals
- Gentle yoga or stretching
- Swimming
- Tai chi or qigong
- Light weight training
Avoid:
- Long-distance running
- High-intensity interval training
- Heavy weightlifting
- Exercise immediately after eating
Natural Supplements That Support Gut Health
Before we dive in: Always talk to your doctor before starting new supplements, especially if you’re taking medications.
Probiotics (Choose Wisely)
Not all probiotics are created equal.
Strains with IBS research:
- Bifidobacterium infantis (reduces inflammation)
- Lactobacillus plantarum (improves gut barrier)
- Saccharomyces boulardii (fights harmful bacteria)
How to take probiotics:
- Start with a lower dose
- Take with food
- Give it 4-6 weeks to work
- Choose multi-strain formulas
Digestive Enzymes (For Better Food Breakdown)
If you feel bloated after every meal, your body might not be producing enough digestive enzymes.
Key enzymes for IBS:
- Amylase (breaks down carbs)
- Protease (breaks down protein)
- Lipase (breaks down fats)
- Lactase (breaks down dairy)
Peppermint Oil (Nature’s Antispasmodic)
Enteric-coated peppermint oil capsules can reduce IBS symptoms by 40-50%.
How it works: Relaxes smooth muscle in the intestines.
Dosage: 0.2-0.4ml three times daily, between meals.
Warning: Can worsen acid reflux in some people.
L-Glutamine (Gut Lining Repair)
This amino acid helps repair and strengthen your intestinal lining.
Dosage: 5-10 grams daily on an empty stomach.
Best time: First thing in the morning or before bed.
When IBS Becomes More Than Just Gut Issues
The Social Impact (The Elephant in the Room)
IBS doesn’t just affect your bathroom habits.
It affects your entire life.
Common social challenges:
- Avoiding restaurants or social events
- Anxiety about traveling
- Feeling embarrassed about symptoms
- Relationships strained by unpredictable symptoms
My advice: Be honest with close friends and family.
You’d be surprised how understanding people can be when you explain what you’re going through.
Work and Career Implications
IBS can seriously impact your professional life.
Workplace challenges:
- Missing important meetings due to symptoms
- Difficulty concentrating when in pain
- Stress about finding bathrooms in unfamiliar locations
- Reduced productivity during flare-ups
Practical solutions:
- Map out bathroom locations in your workplace
- Keep IBS-friendly snacks at your desk
- Practice stress-reduction techniques during the workday
- Consider flexible work arrangements if possible
The Mental Health Connection
The gut-brain axis is real.
When your gut is inflamed, your brain feels it.
Common mental health impacts:
- Depression from chronic pain and unpredictability
- Anxiety about symptoms occurring in public
- Food phobias and eating disorders
- Social isolation and loneliness
This is why I always address both the physical and emotional aspects of IBS in my practice.
Advanced Testing Options for Stubborn Cases
Sometimes basic IBS management isn’t enough.
If you’ve tried diet changes, stress reduction, and supplements without improvement, consider advanced testing.
Comprehensive Stool Analysis
This test analyzes:
- Beneficial bacteria levels
- Harmful bacteria or parasites
- Digestive enzyme function
- Inflammation markers
- Short-chain fatty acid production
Get comprehensive digestive health testing here to understand exactly what’s happening in your gut.
SIBO (Small Intestinal Bacterial Overgrowth) Testing
SIBO occurs when bacteria that should live in your large intestine migrate to your small intestine.
Symptoms that suggest SIBO:
- Bloating within 30 minutes of eating
- Gas that smells like rotten eggs
- Symptoms worse with fiber or probiotics
- Nutritional deficiencies despite good diet
Food Sensitivity Testing
Unlike food allergies (which cause immediate reactions), food sensitivities cause delayed reactions that can last 2-3 days.
Common IBS-triggering sensitivities:
- Gluten (even without celiac disease)
- Dairy proteins (casein, whey)
- Eggs
- Corn
- Soy
My Gut Health Bundle: Everything You Need to Heal Your IBS
Look, I’ve been treating gut issues for years.
And I’ve seen the same story over and over.
People bounce from doctor to doctor.
They try random diets they found on Google.
They take handfuls of supplements without a plan.
And they stay stuck in the same cycle of symptoms.
That’s why I created the Ultimate Gut Health Bundle.
It’s everything I wish I could give every IBS patient in one comprehensive package.
✅ 7-Day Gut Reset Plan
Think of this as your “clean slate.” Each day gives you one clear focus:
- Day 1 – Clean Slate: flushing out the junk that drags your gut down.
- Day 2 – Fiber & Flow: fueling your digestion with the right kinds of fiber.
- Day 3 – Probiotic Power: rebalancing with gut-friendly bacteria.
- Day 4 – Anti-Inflammatory Support: calming irritation and helping your gut heal.
- Day 5 – Mind–Body Reset: reducing stress, which directly affects your digestion.
- Day 6 – Gentle Nourishment: tuning into your body’s signals and giving it what it craves.
- Day 7 – A New Rhythm: setting yourself up for long-term gut-friendly habits.
It’s not overwhelming. It’s not restrictive. Just one step a day — and by the end, your digestion feels lighter, calmer, and more predictable.
✅ Gut Health Worksheet
This isn’t just theory. You’ll have a guided self-assessment with practical questions that help you:
- Spot your gut’s biggest red flags.
- Understand your personal triggers.
- Track progress as you make small, powerful changes.
Most people don’t connect the dots between symptoms and lifestyle. This worksheet makes it crystal clear.
✅ Gut-Friendly Foods Checklist
A quick-reference list of “dos and don’ts” — so you don’t stand in the kitchen wondering what’s safe to eat.
- Foods that naturally support digestion and feed good bacteria.
- Common culprits that secretly irritate the gut.
- Simple swaps you can make to eat smarter without feeling deprived.
Pin it to your fridge and stop second-guessing every meal.
✅ Complete Guide to Gut Health
This is where you finally understand what’s happening inside your body. In plain English, not medical jargon. The guide walks you through:
- Chapter 1: Your Gut is Loaded With Bacteria — how your microbiome works behind the scenes.
- Chapter 2: The Consequences of an Unhealthy Gut — from bloating and fatigue to bigger health risks.
- Chapter 3: Causes of an Unhealthy Gut — the real culprits (it’s not just junk food).
- Chapter 4: Leaky Gut Syndrome — what it is and why it matters.
- Chapter 5: Elimination Diet — how to test foods without losing your mind.
- Chapter 6: Food Allergies vs. Sensitivities — the subtle differences most people miss.
- Chapter 7: Tips for Enhancing Gut Health — practical steps you can start right away.
Get the complete bundle here and start your journey to better gut health today.
The Different Types of IBS (And Why It Matters)
IBS-C (Constipation-Predominant)
What it looks like:
- Fewer than 3 bowel movements per week
- Hard, lumpy stools
- Straining and incomplete evacuation
- Abdominal pain relieved by bowel movements
Treatment focus:
- Increase soluble fiber gradually
- Adequate hydration (half your body weight in ounces daily)
- Gentle movement and exercise
- Magnesium supplements
- Probiotics with Bifidobacterium strains
IBS-D (Diarrhea-Predominant)
What it looks like:
- Frequent loose, watery stools
- Urgency that disrupts daily activities
- Abdominal cramping before bowel movements
- Mucus in stools
Treatment focus:
- Low-FODMAP diet
- Avoid trigger foods (caffeine, alcohol, spicy foods)
- Stress management techniques
- Peppermint oil supplements
- Probiotics with Lactobacillus strains
IBS-M (Mixed Type)
What it looks like:
- Alternating between constipation and diarrhea
- No predictable pattern
- The most challenging type to manage
Treatment focus:
- Comprehensive approach addressing both constipation and diarrhea
- Careful attention to trigger identification
- Flexible treatment plan that adapts to symptoms
- Strong focus on stress management
Common IBS Myths (That Keep You Stuck)
Myth #1: “IBS Is Just Stress”
Reality: Stress can trigger symptoms, but IBS has real physical causes.
Your gut bacteria, immune system, and nervous system are all involved.
Dismissing IBS as “just stress” prevents proper treatment.
Myth #2: “You Just Need More Fiber”
Reality: The wrong type of fiber can make IBS worse.
Insoluble fiber (like wheat bran) can increase symptoms.
The key is finding the right type and amount for your body.
Myth #3: “IBS Will Turn Into Something Worse”
Reality: IBS doesn’t increase your risk of colon cancer or inflammatory bowel disease.
It’s a functional disorder, not a structural disease.
While uncomfortable, IBS doesn’t damage your intestines.
Myth #4: “There’s Nothing You Can Do About IBS”
Reality: IBS is highly manageable with the right approach.
Most people can significantly reduce symptoms with diet, lifestyle changes, and targeted supplements.
The key is finding what works for your specific type of IBS.
Creating Your Personal IBS Action Plan
Week 1-2: Assessment and Baseline
Goals:
- Track all symptoms and triggers
- Establish baseline bowel habits
- Identify major stress sources
Actions:
- Start a detailed symptom diary
- Take photos of your stools (I know it’s weird, but it’s helpful)
- Rate your stress levels daily (1-10 scale)
- Note sleep quality and energy levels
Week 3-4: Eliminate Obvious Triggers
Goals:
- Remove the most common IBS triggers
- Establish better stress management habits
- Improve sleep hygiene
Actions:
- Eliminate caffeine, alcohol, and artificial sweeteners
- Start a 10-minute daily meditation practice
- Establish consistent sleep and wake times
- Begin gentle exercise routine
Week 5-8: Targeted Dietary Changes
Goals:
- Identify specific food triggers
- Establish a sustainable eating pattern
- Begin supplement protocol
Actions:
- Try low-FODMAP diet for 4-6 weeks
- Reintroduce foods systematically
- Add targeted supplements (probiotics, digestive enzymes)
- Continue stress management practices
Week 9-12: Fine-Tuning and Optimization
Goals:
- Optimize successful strategies
- Address remaining symptoms
- Build long-term habits
Actions:
- Adjust diet based on reintroduction results
- Fine-tune supplement protocol
- Consider advanced testing if needed
- Plan for long-term maintenance
Building Your IBS Support System
Healthcare Team Assembly
Primary care physician:
- Initial diagnosis and basic management
- Referrals to specialists
- Medication management
Gastroenterologist:
- Advanced diagnostic procedures
- Complex case management
- Medication options
Registered dietitian:
- Personalized nutrition plans
- Food sensitivity identification
- Meal planning support
Mental health professional:
- Stress management techniques
- Cognitive behavioral therapy
- Anxiety and depression treatment
Family and Friends Support
How to explain IBS to others:
- Be honest about the unpredictability
- Explain that symptoms are real, not imaginary
- Ask for specific support (flexibility with plans, understanding about food choices)
- Share educational resources
Online Communities and Resources
Benefits of IBS support groups:
- Connect with others who understand your experience
- Share practical tips and strategies
- Reduce feelings of isolation
- Learn about new treatments and research
Recommended resources:
- International Foundation for Gastrointestinal Disorders
- IBS support groups on Facebook and Reddit
- Local hospital support groups
- IBS-specific apps for tracking symptoms
The Future of IBS Treatment
Emerging Research Areas
Microbiome therapy:
- Fecal microbiota transplantation (FMT) for severe cases
- Targeted probiotic strains
- Prebiotic supplements to feed beneficial bacteria
Personalized medicine:
- Genetic testing to predict treatment response
- Microbiome analysis for targeted interventions
- Biomarker identification for earlier diagnosis
New medications:
- Gut-specific antibiotics
- Serotonin receptor modulators
- Anti-inflammatory agents
Technology and IBS Management
Apps and digital tools:
- Symptom tracking applications
- AI-powered dietary recommendations
- Telemedicine for ongoing care
- Meditation and stress management apps
Wearable devices:
- Heart rate variability monitoring for stress
- Sleep quality tracking
- Activity monitoring for exercise optimization
Your Next Steps: Taking Action Today
If you’ve made it this far, you’re serious about addressing your IBS symptoms.
Here’s what I want you to do right now:
Immediate Actions (Next 24 Hours)
- Start a symptom diary Download a notes app or grab a notebook Track everything you eat, drink, and feel for the next week
- Schedule a doctor’s appointment If you haven’t been formally diagnosed, get proper medical evaluation Rule out other conditions that mimic IBS
- Begin stress reduction Start with 5 minutes of deep breathing today Download a meditation app Take a 10-minute walk outside
This Week
- Clean up your diet Eliminate obvious triggers (caffeine, alcohol, processed foods) Focus on simple, whole foods Stay hydrated
- Improve sleep hygiene Set a consistent bedtime Remove screens from bedroom Keep room cool and dark
- Get my Gut Health Bundle Download it here for a complete, step-by-step plan Start with the 7-Day Gut Reset Use the worksheet to identify your personal triggers
This Month
- Try the low-FODMAP diet Work with a dietitian if possible Follow the elimination phase for 4-6 weeks Systematically reintroduce foods
- Add targeted supplements Start with a quality probiotic Consider digestive enzymes if you have bloating Try peppermint oil for cramping
- Consider advanced testing Get comprehensive digestive testing if basic approaches aren’t helping Look into SIBO testing if you have severe bloating Consider food sensitivity testing
Frequently Asked Questions About IBS Signs
Q: How long does it take to see improvement in IBS symptoms?
A: Most people notice some improvement within 2-4 weeks of making dietary and lifestyle changes.
However, full symptom management can take 2-3 months.
The key is consistency and patience.
Your gut didn’t get this way overnight, and it won’t heal overnight either.
Q: Can IBS symptoms come and go, or are they constant?
A: IBS symptoms are typically episodic.
You might have weeks or months of minimal symptoms, followed by flare-ups.
This unpredictability is actually one of the hallmark signs of irritable bowel syndrome.
Triggers like stress, certain foods, or hormonal changes often precipitate flare-ups.
Q: Is it normal to have mucus in stool with IBS?
A: Yes, mucus in stool is very common with IBS.
Your inflamed intestinal lining produces extra mucus as a protective mechanism.
However, if you notice blood mixed with the mucus, see a doctor immediately.
Blood in stool is not a normal IBS symptom and requires evaluation.
Q: Can children develop IBS, or is it only an adult condition?
A: Children can absolutely develop IBS.
In fact, many adults with IBS report their symptoms started in childhood or adolescence.
Signs in children include recurring stomach pain, changes in bowel habits, and bloating.
If your child has persistent digestive symptoms, consult their pediatrician.
Q: Are there any foods that universally trigger IBS symptoms?
A: While triggers are highly individual, some foods commonly cause problems:
- High-FODMAP foods (onions, garlic, beans, certain fruits)
- Dairy products (if lactose intolerant)
- Gluten-containing grains
- Artificial sweeteners (sorbitol, mannitol)
- Caffeine and alcohol
- Spicy or very fatty foods
The key is identifying YOUR specific triggers through careful tracking.
Q: Can stress alone cause an IBS flare-up?
A: Absolutely.
Stress is one of the most common triggers for IBS symptoms.
The gut-brain connection is so strong that emotional stress can immediately affect gut function.
This is why stress management is a crucial part of IBS treatment.
Q: How do I know if my symptoms are IBS or something more serious?
A: See a doctor immediately if you have:
- Blood in your stool
- Unexplained weight loss
- Fever with digestive symptoms
- Severe pain that doesn’t improve
- Symptoms that wake you from sleep
IBS symptoms, while uncomfortable, don’t typically include these “red flag” signs.
Q: Can probiotics make IBS symptoms worse?
A: Yes, some people with IBS actually feel worse when they start probiotics.
This can happen if you have SIBO (small intestinal bacterial overgrowth) or if you’re taking the wrong strains.
Start with a low dose and choose strains specifically researched for IBS.
If symptoms worsen, stop and consult your healthcare provider.
Q: Is IBS hereditary? Will I pass it to my children?
A: There is a genetic component to IBS, but it’s not directly inherited like eye color.
If you have IBS, your children have a higher risk of developing it, but it’s not guaranteed.
The risk comes from a combination of genetics, shared environment, and learned behaviors around food and stress.
You can reduce your child’s risk by modeling healthy eating habits and stress management techniques.
Q: Can hormone changes affect IBS symptoms?
A: Yes, especially for women.
Many women notice their IBS symptoms fluctuate with their menstrual cycle.
Estrogen and progesterone levels affect gut motility and pain sensitivity.
Symptoms often worsen during menstruation and may change during pregnancy or menopause.
Birth control pills and hormone replacement therapy can also impact symptoms.
Q: How accurate are at-home IBS tests?
A: At-home tests can provide useful information, but they shouldn’t replace proper medical evaluation.
Tests like food sensitivity panels and microbiome analysis can offer insights, but they need to be interpreted by a healthcare professional.
Advanced digestive testing through reputable labs can be valuable for identifying underlying issues.
Always discuss results with your doctor before making major treatment changes.
Q: Can exercise make IBS symptoms worse?
A: High-intensity exercise can worsen IBS symptoms, especially during a flare-up.
However, gentle, regular exercise usually improves symptoms by:
- Reducing stress
- Improving gut motility
- Strengthening the gut-brain connection
Best exercises for IBS include walking, yoga, swimming, and light strength training.
Avoid intense workouts immediately after eating.
Q: Is there a cure for IBS, or is it a lifelong condition?
A: Currently, there’s no cure for IBS, but it’s highly manageable.
Many people achieve near-complete symptom control through diet, lifestyle changes, and stress management.
Some people find their symptoms naturally improve over time, especially as they learn to manage triggers effectively.
The goal isn’t necessarily to “cure” IBS, but to live symptom-free most of the time.
Q: Can IBS cause weight loss or weight gain?
A: IBS can contribute to both weight loss and weight gain, depending on your symptoms and coping strategies.
Weight loss can occur from:
- Diarrhea-predominant IBS causing malabsorption
- Food restriction due to fear of triggering symptoms
- Loss of appetite during flare-ups
Weight gain can result from:
- Constipation and bloating
- Emotional eating during stressful periods
- Choosing processed “safe” foods that are high in calories
If you’re experiencing significant weight changes, work with a healthcare provider and dietitian.
Q: Can certain medications trigger or worsen IBS?
A: Yes, several medications can trigger IBS symptoms:
Antibiotics disrupt gut bacteria balance NSAIDs (ibuprofen, naproxen) irritate the intestinal lining Antidepressants can affect gut motility Birth control pills may influence symptoms through hormonal changes Artificial sweeteners in medications can trigger symptoms
Never stop prescribed medications without consulting your doctor, but discuss alternatives if you suspect a medication is worsening your IBS.
The Bottom Line: Your Journey to Better Gut Health Starts Now
Look, I’ve thrown a lot of information at you.
But here’s what I want you to remember:
The signs of irritable bowel syndrome don’t have to control your life.
You’re not broken.
You’re not imagining things.
And you’re definitely not alone.
IBS affects millions of people, and the vast majority find ways to manage their symptoms effectively.
The key is taking action.
Not tomorrow. Not next week. Today.
Start with small changes:
- Track your symptoms for one week
- Eliminate one obvious trigger
- Practice deep breathing for 5 minutes daily
- Download my Gut Health Bundle for a complete roadmap
Remember, healing isn’t linear.
You’ll have good days and bad days.
But with the right approach, the good days will start outnumbering the bad ones.
Your gut has an amazing ability to heal.
Give it the support it needs, and you might be surprised at how much better you can feel.
The signs of irritable bowel syndrome brought you here today.
Now let them guide you toward better health.
Ready to take control of your gut health? Get my complete Gut Health Bundle and start your healing journey today. For advanced testing to understand exactly what’s happening in your digestive system, check out comprehensive digestive health testing options here.